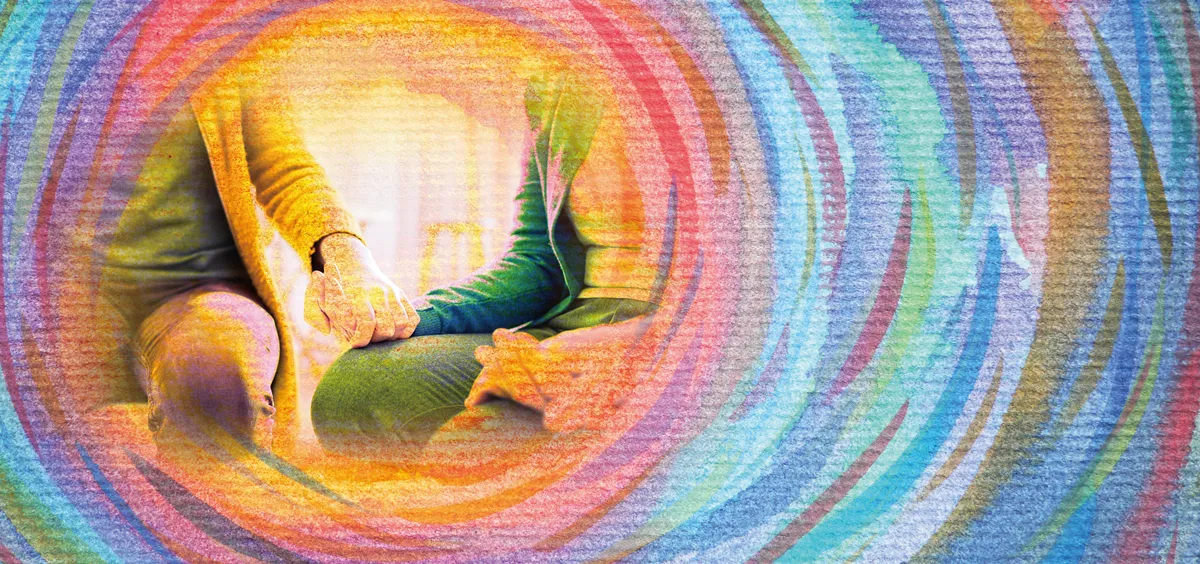
Rehabilitation for mental illness, still rare in China, provides a bridge between hospitalization and society
Rhododendrons, peonies, roses: On the fourth floor patio, counselor Chen Hengsheng hands out rubber gloves to prepare mulch in order to move the flowers, still in their pots, into the planters.
The gardeners are members of Hope Clubhouse, a community rehabilitation center for persons with mental illnesses in Chengdu, Sichuan province. On a Monday morning, Chen and five other full-time counselors greet clubhouse members warmly as they enter.
For seven years, Shen Yu has kept up perfect attendance every weekday. She tells TWOC that she previously worked in a call center for over a decade, until one day she felt suddenly lifeless, and could no longer muster the energy to go to work. “I would cry, yell, and smash things.” When her husband, a railway technician, left for another long business trip, her condition deteriorated. Her family brought her to the hospital, where she was diagnosed with schizophrenia.
Discharged from a month-long hospital stay, Shen was warned by her doctor that being home alone could allow her condition to worsen. After leaving the hospital in 2013, she was referred to Hope Clubhouse by her doctor, and has continued coming since.
Rehabilitation centers like Hope Clubhouse seek to turn the page on the treatment of China’s 16 million people living with severe mental illnesses, including 7 million people living with schizophrenia.
In 2003, following the SARS epidemic, China’s central government launched one of the world’s most ambitious demonstration programs to expand basic mental health care coverage to neighborhoods. By the end of 2012, over 249,000 patients received free outpatient treatment and 40,000 had received free inpatient care in 60 demonstration sites across the country in what became known as the “686 Program.”
China has since strived to fill in what the Ministry of Health calls “blank areas” with total lack of mental health care coverage, comprising 41.9 million people in 2006. Psychiatric departments in universities, a profession discredited in the Mao era, reopened and expanded in the 1980s, churning out personnel for severely understaffed hospitals around the country. However, by 2015, two-thirds of counties still did not have a single psychiatrist.
Clubhouses seek to break the loneliness of recovery
Before the 686 Program, much of China’s mentally ill population was invisible. At its most extreme, healthcare workers responsible for registering participants for the program reported finding over 250 people with schizophrenia who had been restrained in their homes between 2005 and 2009, for periods ranging from two weeks to 28 years.
In 2010, Chinese media reported the story of Xiaobin, a 21-year-old man in Anhui province who had been kept chained to a wooden barrel for two years. Xiaobin’s family had been unable to afford his treatment for schizophrenia (it was estimated that 57 percent of those with severe mental disorders in China lived below the official poverty line in 2014), and had to chain him in the home for his own safety and that of his neighbors.
While such stories were met with widespread shock and condemnation, it became clear that families without resources to rehabilitate their loved ones resorted to dire measures for lack of better alternatives. In a study by Peking University and Harvard Medical School published in 2015, 96 percent of respondents cited “financial difficulties,” and 87 percent cited “no capable caretaker,” as the main reasons for forcefully restraining their family members.
A follow-up study found that under an intensive track of the 686 Program’s treatment, three in four of the 266 formerly restrained patients took regular medication, 79 percent improved their social functioning, and 92 percent stayed free of restraints in 2012.
Although the program registered less than 1 in 3 people estimated to live with severe mental illnesses in China, the message was powerful—persons with severely mental illnesses can lead hopeful lives, and need sustained access to medicine and support.
“The mental health system reform in China has entered a critical period,” wrote a team led by Jianyu Que of Peking University Sixth Hospital, the country’s preeminent psychiatric hospital, in a 2019 scientific paper. The authors concluded that a rehabilitation system is necessary to “prevent disability and poverty caused by mental disorders and promote the re-entry of patients into society.”
Health and emotional management lessons fill dire gaps in mental health education
Rehabilitation can be an arduous process, especially for those without full-time caretakers. “At the time, the side effects of my medication were serious,” Shen recalls. “It didn’t feel right to sit, or to stand; it was very painful. I felt that life was more painful than death.”
To help adjust to her medication, Shen came to the clubhouse daily, where she received free one-on-one counseling, worked in the food services unit, and participated in activities. “It’s hard for people to rediscover their place in life. The stage after hospital treatment, of returning home, is crucial,” says Dr. Zhang Shusen, a psychiatrist at West China Hospital and part of Hope Clubhouse’s founding team.
Yet community-based mental health rehabilitation centers in China remain few and far between. Some of the first and most enduring organizations in China have followed the “clubhouse model” based on a psychosocial rehabilitation center founded in New York City in 1943. In contrast to a psychiatric hospital, where stays can be involuntary and costly, the clubhouse conceived of participation that is entirely voluntary, free of charge, and never expires.
Participants are “members” rather than “patients,” and clubhouse activities focus on building their strengths and abilities, instead of on their illness. Members perform duties in administration and food services, and take part in programs including vocational training and emotional management. Just as importantly, they celebrate birthdays together, garden together, and form meaningful relationships that support them through recovery.
The model has spread to over 30 countries. The first clubhouse in Hong Kong opened in 1998, and the first on the Chinese mainland opened in Hunan province in 2007. Six clubhouses recognized by the NGO Clubhouse International now operate on the mainland, four of which have passed accreditation for professional standards.
Clubhouse members and staff “work shoulder-to-shoulder,” says Shen. “In some ways, our relations are better than with family. Sometimes people like us don’t get along with our actual family.”
In a mental health system still severely strained for staff and resources, clubhouses fill a crucial gap between hospital stays and neighborhood care. However, the development of clubhouses in China “has not been smooth,” according to Dr. Zhang.
Dr. Zhang conjectures that the first mainland clubhouse in Hunan province received enthusiastic support from the provincial government, leading to the rapid growth of a number of clubhouses in the province. However, many in smaller cities remain substandard for lack of local psychological expertise, making doctors hesitate to refer their patients.
Working in the food services team provides social connection and support to clubhouse members
Meanwhile, the clubhouse in Kunming, the capital of Yunnan province, grew from grassroots efforts and has virtually no budget for staff training, affecting its services and fettering its growth. A successful clubhouse requires cooperation between numerous local government bureaus, hospital staff, and civil society—a difficult balance to strike.
With barebones funding and facilities, the work remains an uphill battle. One constant and enduring obstacle is deeply entrenched stigma from neighborhoods, families, and even patients themselves. A 2019 study spearheaded by Luming Li of Yale University Psychiatric Hospital quotes a counselor in Hunan province who says that neighbors have asked his clubhouse to move out of the community, as they are afraid that the patients might be dangerous.
“Society seems to treat having a mental illness as worse than committing a crime,” says Chen, the counselor at the Chengdu clubhouse, whose experience with an uncle with schizophrenia partially motivated him to work at the rehabilitation center. “Some people say that stealing and snatching are better than getting a mental illness, because at least your children cannot inherit it. Many people think once you are diagnosed, your life is over.”
Chen says after being diagnosed with a severe mental illness, patients may be disqualified from buying private health insurance, contributing to their reluctance to seek help.
Many families prefer to care for their mentally ill relatives at home, either finding mental illness shameful, or mistrusting institutions to provide adequate care. “Doctors need to bring patients to the clubhouse sometimes,” says Dr. Zhang. “When people find out that they have other illnesses, they are eager to cure it. When they find out they have a mental illness, they deny it, find it embarrassing, and just say that they are unhappy.”
The role of family is both a blessing and a curse for patients. While over a quarter of the 100,000 to 200,000 chronically homeless in the US suffer from a serious mental illness, the chances of people with mental illnesses becoming homeless is thought to be much lower in China due to tighter-knit families. On the other hand, people with mental illnesses are often kept within the home.
Even as mental health awareness increases, and more patients than ever are accessing China’s growing network of psychiatrists, rehabilitation remains the missing link. A study in Sichuan province found that of 2,757 people diagnosed with schizophrenia who passed away between 2011 and 2013, only 1 percent of them were actively receiving treatment in the period before their death. Upon leaving the hospital ward, patients are often out of sight and out of mind, but recovery requires sustained follow-up care.
Computer skills and vocational training help clubhouse members return to the workforce
It is increasingly clear that hospitals alone cannot safeguard a patient’s recovery. “Over-prescription is a worrying trend,” Daniel Vuillermin, lecturer at Peking University’s School of Health Humanities, tells TWOC. At understaffed hospitals, psychiatrists who have little time for lengthy consultations rely largely on prescribing drugs to treat patients. A study lead by Yu Zhenwei of Zhejiang University showed that from 2013 to 2018, prescription rates of anti-depressants increased by 43 percent in six major Chinese cities.
Vuillermin explains that the approach of “throwing medication at people” glosses over the importance of social and environmental factors of illness. Rehabilitation must calibrate not only chemical imbalances in the brain, but family and social relationships. While doctors look at the biological elements of treatment, rehabilitation looks at the social factors.
Indeed, many of the clubhouse’s members tell of extreme pressures in work, school, and family, which can often trigger biological and physical predispositions to mental illness. One member stated she fell ill after disputes with a developer that ended in her neighborhood being demolished.
Clubhouses teach techniques for emotional regulation and health, as well as provide one-on-one counseling and peer support through working in a team. At the center of community rehabilitation is the idea that in order to return to regular life, one must recreate a sense of belonging: first by finding a supportive community, and then, ideally, transitioning back to work and school.
Members who are ready are encouraged to participate in the transitional employment program. The Chengdu clubhouse collaborates with a dozen international and Chinese companies; members are hired for part-time positions, and the clubhouse guarantees that if employees don’t show up to work, they will provide a replacement worker.
However, while international companies have an established practice of corporate social responsibility, there is little precedent among Chinese companies for specialized hiring. Compared to similar programs in the US, the program in Chengdu is mostly limited to a handful of companies brought on through personal connections.
Nevertheless, those who go through the program benefit from the independence and self-worth of supporting oneself and one’s family. An 18-year-old clubhouse member who learned computer skills at the clubhouse enrolled in the transitional employment program, where he gained the confidence to find another job at a business selling computers.
Another program seeks to help students who have dropped out for mental health reasons to return to school and rehabilitate their relationship with their parents. “Chinese parents love their kids so much, but are indirect to the point that their children cannot see it. Or they are anxious and critical,” explains Gao, a project consultant for the Chengdu clubhouse who specializes in child and family therapy. “Unfortunately, some children develop mental illness before their parents can see problems with their thinking.”
The clubhouse model has received a spate of recognition from central government. The State Council used the Changsha clubhouse as an example in its 2013 case book on social management innovation for mental illness, which provides recommendations for local and national governments to adopt. In 2017, the Ministry of Civil Affairs noted the clubhouse model in an opinion document to accelerate the development of community-based rehabilitation services. In 2019, the Specialized Committee of Mental Health Rehabilitation was founded, the first national institution aimed at promoting psychiatric rehabilitation.
However, community rehabilitation centers need not only political will, but funding. “The government has documents, which provide a framework, but you need people to execute it,” Dr. Zhang notes. “We need not only policies, but also personnel.”
Full-time staff at the Chengdu clubhouse are paid about 4,000 RMB a month with social benefits, hardly a competitive salary for a licensed counselor. “They can work on compassion for some time, but we’ve all got to live,” Dr. Zhang sighs.
The afternoon rays warm the patio of the clubhouse on a rare sunny day in Chengdu. Everyone seems glad to be outside, gradually turning piles of dirt on a concrete slab into a verdant garden. Counselor Chen is leading the project, having brought his own flowers from home for transplantation.
“If you’re a gardener, you’d understand our work,” says Chen. “Flowers need to adjust to their surroundings. Don’t people, too?”
Cover illustration by Cai Tao, Elements from VCG; Other photographs by Hope Clubhouse Chengdu
House of Hope is a story from our issue, “You and AI.” To read the entire issue, become a subscriber and receive the full magazine.